The Emerging Role of AI-Driven Virtual Care in Revolutionizing Healthcare Delivery
Healthcare is undergoing a rapid transformation propelled by artificial intelligence (AI), telehealth, and data-driven ecosystems. A subtle but disruptive weak signal lies in the integration of AI-driven virtual care solutions into mainstream healthcare, potentially redefining how care is delivered, accessed, and managed. This development could reshape multiple sectors, from healthcare providers and insurers to technology companies and policymakers, creating both opportunities and complex challenges over the next two decades.
Introduction
AI-based virtual care is advancing beyond simple telehealth communications, combining remote patient monitoring, intelligent automation, and disease analytics to create comprehensive, proactive healthcare ecosystems. This shift also coincides with regulatory changes promoting telehealth utilization and expanding care accessibility. Together, these trends could transform healthcare from reactive episodic treatment to continuous, anticipatory management with significant downstream effects across economics, clinical outcomes, and healthcare equity.
What’s Changing?
Recent developments suggest a convergence of technology, policy, and investment driving a new paradigm in healthcare delivery:
- AI-Driven Virtual Care Expansion: Companies like MiCare Path are accelerating the national adoption of AI-enabled virtual care platforms to provide personalized chronic disease management and remote patient monitoring (TechStartups, 2025). This indicates a shift from basic telehealth visits to integrated, AI-powered care coordination that can detect early warning signs and guide intervention.
- Telehealth as Core Healthcare Modality: The Centers for Medicare & Medicaid Services (CMS) have permanently lifted limits on telehealth service frequencies in inpatient and nursing settings, normalizing virtual care as an essential healthcare access tool (Arnold & Porter, 2025). This regulatory evolution could significantly expand telehealth demand and utilization.
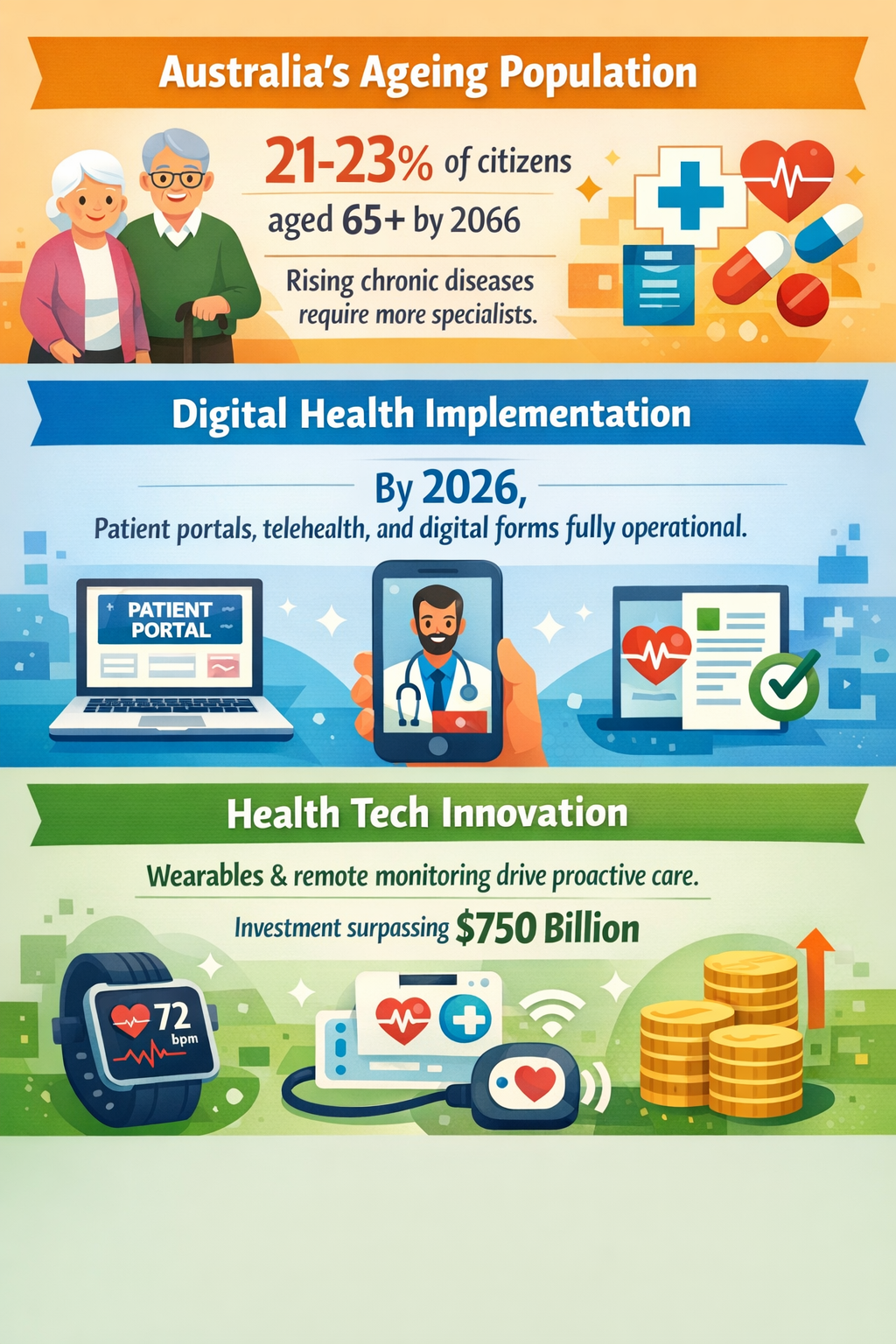
- Proactive and Data-Driven Care Models: Investment exceeding $750 billion is flowing into digital health innovations like wearables and remote monitoring, creating ecosystems that enable continuous health data collection alongside AI analytics (BioSpace, 2025). These systems are positioned to move healthcare from reactive to proactive models.
- Technological Acceleration in Remote and Emergency Care: Innovations exemplified by initiatives such as Queensland’s telehealth-enabled emergency response and advanced surgical access through robotic assistance reflect increased capabilities for delivering critical and specialist care remotely (C-MW.Net, 2025).
- Addressing Chronic Disease with AI-Supported Prevention: Chronic diseases pose enormous economic and social costs, but AI virtual care systems could improve management and prevention by early detection of risk factors and patient-specific interventions, potentially preventing millions of cases and reducing trillions in costs (Fight Chronic Disease, 2024).
- Mental Health Services Expansion via Telehealth: The growing integration of telepsychiatry into virtual health platforms meets increasing demand for accessible mental healthcare, especially in urban regions like Los Angeles, demonstrating the breadth of ailments AI virtual care could address (BrainHealthUSA, 2025).
The common thread running through these changes is the maturation of AI virtual care into a multifaceted ecosystem that exceeds simple telehealth encounters, blending data, automation, and machine learning to create a continuously learning system capable of more personalized, efficient, and scalable healthcare delivery.
Why is this Important?
The transition towards AI-driven virtual care could have profound impacts:
- Cost Efficiency and Disease Prevention: Chronic diseases including obesity impose a trajectory of escalating costs and mortality. AI-enabled early intervention and management systems may reduce the incidence and severity of these conditions substantially, producing national savings estimated in the trillions (Fight Chronic Disease, 2024).
- Healthcare Access and Equity: Removing frequency caps on telehealth and expanding digital health platforms can improve access for rural, disabled, and mobility-constrained populations, thereby addressing longstanding geographic and socioeconomic disparities (Arnold & Porter, 2025; Abilities, 2025).
- Operational Transformation for Providers: Intelligent automation is projected to become the fastest-growing healthcare segment, improving workflow efficiency, real-time disease monitoring, and decision support, enabling providers to focus resources where human judgment adds most value (2AM.Tech, 2025).
- New Industry Collaborations and Markets: The overlap of healthcare providers, technology developers, and regulators in AI virtual care ecosystems signals new partnership models and competitive landscapes, potentially disrupting traditional healthcare business models and vendor relationships (TechStartups, 2025).
- Data Privacy and Regulation Challenges: Expanding remote and AI-driven care will escalate issues around patient data sovereignty, cybersecurity risks, and ethical AI usage, demanding nuanced policy responses to balance innovation with protections.
Implications
Foresight into the continuing evolution of AI-driven virtual care suggests several critical considerations for stakeholders:
- Providers and Health Systems: Should accelerate adoption and integration of AI virtual care platforms to improve patient outcomes and reduce costs, while training staff to leverage AI insights effectively. Preparation for interoperability and data governance will be key.
- Technology Developers: Need to refine AI algorithms toward explainability, bias reduction, and multi-condition management to build trust and broad adoption. Collaboration with clinical experts and regulators will support safer, validated solutions.
- Policymakers: Must evolve regulatory frameworks to manage telehealth permanency, data security, reimbursement models, and cross-jurisdictional licensing to sustain inclusive and ethical growth.
- Insurers and Payers: Could explore adaptable reimbursement strategies to incentivize preventive virtual care services and align financial incentives with long-term health gains.
- Patients and Caregivers: Will increasingly engage with digital health tools, necessitating support for health literacy and digital inclusion to avoid exacerbating disparities.
- Academic and Research Institutions: Should monitor real-world AI virtual care outcomes and ethical impacts continuously, providing evidence to refine innovation pathways and policies.
The pace and scale of transformation may create unintended consequences; stakeholders will need to balance enthusiasm for AI-enabled possibilities with vigilant risk management and stakeholder dialogue to realize a positive, win-win healthcare future.
Questions
- How can healthcare organizations integrate AI virtual care without compromising clinical quality and patient trust?
- What regulatory frameworks are needed to safeguard data privacy and ensure equitable access while fostering innovation?
- How might payment models evolve to reward preventive, AI-driven remote care and chronic disease management?
- What strategies can minimize bias and ensure AI algorithms serve diverse patient populations fairly?
- How will the patient-provider relationship change as AI moderates more care decisions, and what new ethical considerations arise?
- Which cross-sector partnerships are essential to building sustainable AI virtual care ecosystems?
- What infrastructure investments in broadband and technology access will be necessary to prevent digital health inequalities?
Keywords
AI virtual care; telehealth; remote patient monitoring; chronic disease management; digital health ecosystems; intelligent automation healthcare; healthcare policy regulation
Bibliography
- Better prevention, earlier intervention, and improved management of chronic disease, especially obesity, could prevent 150 million new chronic disease cases, save 13.5 million lives, and avoid $7 trillion in costs nationally between 2024 and 2039. Fight Chronic Disease, 2024
- Healthcare is expected to see the fastest growth by 2030, as intelligent automation helps improve patient care, enable real-time disease analysis, and expand telehealth services. 2AM.Tech, 2025
- Queensland is already a global leader in telehealth-enabled emergency response, and CAOS 2028 will further accelerate innovation to make advanced surgical care more accessible than ever. C-MW.Net, 2025
- Digital health innovation from wearables to remote patient monitoring are pushing care models toward proactive, data-driven ecosystems, backed by investment expected to surpass US$ 750 billion. BioSpace, 2025
- The latest funding-and-acquisition move will accelerate MiCare Path's national expansion and bolster its AI-driven virtual care solutions at a time when healthcare providers are increasingly adopting telehealth and remote patient monitoring. TechStartups, 2025
- CMS will permanently remove frequency limitations for how often telehealth may be used with regard to subsequent care services in inpatient and nursing facility settings, as well as for critical care consultation services. Arnold & Porter, 2025